Inside the Red Zone
2020
May
18
They drafted the operations manual of the coronavirus treatment centre in a weekend, including its precise parameters, prerequisites and guidelines. An out-of-use building of the Baranya County Hospital has been chosen as the location, which has been last used as an ICU 5 years ago. This is how the 4th floor of building “C” became the Intensive Care Unit of the Coronavirus Care Centre (KEK), which has been set up within days with the support of the UP Operative Crew. We interviewed Dr. Tamás Kiss, the head of the Covid-ICU and his deputy, Dr. Krisztián Jáksó. The marks left by the protective masks have been still visible on their faces.

Who are treated at the Covid-ICU?
Patients with a confirmed or suspected infection, who suffer from respiratory/ cardiovascular distress need intensive therapy. The majority of our patients have not been confirmed COVID-19 positive, although they showed symptoms similar to coronavirus infection and they needed intensive care. After two negative results, they can be transferred to other units of the Clinical Centre. This ICU had to be set up in order to treat confirmed as well as suspected positive patients.

How many people have recovered so far?
Thankfully, we had relatively few patients altogether, all have been treated, and we have seen recoveries too.

If somebody has to be put on a ventilator, what can you do for them?
Dr. Tamás Kiss: These steps of intensive therapy are basically categorized as organ support therapies. Ventilation is a form of treatment, which relieves the body and assists the respiratory system in order to enable it to heal. Further treatment is carried out according to a set procedure. It is true unfortunately, that we cannot help everyone, although we desperately want to.
Dr. Krisztián Jáksó: We do not have an actual vaccine against COVID-19, but we do have about 200 substances, which are tested currently. These substances were not created to treat this disease, however, they might be effective or they might slow down the spreading of the virus within the body. This means, that our patients receive all those drugs that are given to patients all over the world. We apply those drugs, which might possibly work against the virus. If one among three substances works or can slow down the spreading of the virus, that is good, because it can give the patient some time. Vaccination, which will be the solution, can take a longer time to be developed.

How can the relatives of patients receive news about their loved-ones?
Dr. Tamás Kiss: Personal visits are not possible at the moment, we can only give information on the phone after appropriate verification. We also made a decision that only doctors are allowed to give information, and we also ask for double verification: the relatives on the phone have to identify themselves and the patient as well.

This unit had to be established within only a couple of days. Was it difficult to find experts, colleagues for a challenge like this?
Dr. Tamás Kiss: The Operative Crew of the university has done everything in their power to meet the conditions necessary for the establishment and successful operation of a department like this. Everything went very smoothly from licences to purchasing instruments and building walls.
Dr. Krisztián Jáksó: 22 doctors from the Department of Anaesthesiology and Intensive Therapy volunteered to work in the Coronavirus Care Centre.
We both are proud of this; they are all working in shifts for the positive patients.

How can you prepare in advance for the flood of patients that might arrive any minute?
Dr. Tamás Kiss: Our colleagues from abroad, with whom we keep in touch from the UK primarily, say that until you are living in it, it is impossible to imagine, what the situation is like. Just to mention an example: our British colleagues had one nurse for one patient on average, now one nurse might be required to care for up to six patients. This is simply unprecendented. In Hungary, we do not know either, how the situation might escalate.
We try to be prepared.
So far, I have to say, although there are relatively few patients, that our unit has done well. Proof of that is, that none of our staff got infected, although we are treating confirmed COVID-19 patients at the intensive care unit.

What are the shifts like at the Coronavirus Care Centre?
Dr. Krisztián Jáksó: The doctors are working in on-call-system, the nurses are working in shifts. The doctor on-call is here for 24 hours, if they are not on call, then they go home after 8 or 12 hours. The nurses are working in 12-hour shifts.
We can spend maximum three hours in the red zone, then a rest is required, which is relative, but it does not mean doing nothing,
because the colleagues have to take part in consultations, resuscitations, restocking supplies nevertheless.
Why is the limit in the red zone set in 3 hours?
Dr. Krisztián Jáksó: We have decided that this would be the limit, because that is still manageable psychologically and physically. It is more difficult to breathe through the mask, which can get exponentially more difficult, it depends on your habitude and lung capacity. It is not child’s play to work three hours more than once a day in protective gear. We are proud that our colleagues are doing great.
To be in the red zone while there are patients who are potentially infectious is different from when we practised a similar situation in the Medical Simulation Education Center.
The system passed the initial “test”, there were no serious accidental mistakes – anyone can get sick, or can have an asthma attack, or they can unintentionally touch their nose or adjust their glasses, etc…
Dr. Tamás Kiss: International recommendation prescribe a limit of 4 hours. We decided on a limit of 3 hours, in adjustment to the schedules of the department, keeping in mind that we have to make the right decisions quickly, wearing protective suit and masks as well.

Everything is disinfected, and everyone knows how important it is to behave responsibly. From the point of view of getting infected is the COVID-ICU (KEK ITO) one of the safest places in Pécs?
Dr. Tamás Kiss: Yes, we think so. If we use the protective gear appropriately and follow the rules, there is a lower chance to catch the virus here, than in a shopping mall or on the market.
We have to take the epidemiological regulations seriously!
It is for sure that one of the reasons for a flatter epidemic curve in Hungary are these precautions.
Dr. Krisztián Jáksó: All of us go home from this place to our families, children, parents with a deeper feeling of security, than from a shopping centre, or just the streets. We are planning to write a book about our personal experiences with the title: The Big 2020 IQ Test.

Is it a challenge to manage the COVID-ICU?
Dr. Tamás Kiss: It is not easy, that is for sure. You have to pay attention not only to professional perfectionism, but to many other factors as well. You have to be present everywhere more or less. You always have to spend time with the colleagues, which is more necessary now than ever. Our main job is to follow the rules and standards at all times without fail and to make everyone do the same.
We are lucky that in this unlucky situation, we had the chance to develop and to adapt the systems thanks to the flatter curve. We are used to making responsible decisions quickly. In the first 2-3 weeks, we definitely slept less than usual, but I see that we are getting used to the system.

What can everyday people do to help?
Dr. Tamás Kiss: For now, stay at home! Individually there is a relatively smaller chance of getting seriously ill. However, society has to pay attention to those, who have certain health problems, because they are more vulnerable, and we can pass the infection on to them without noticing any symptoms on ourselves. This epidemic has spread all over the world, because many people infected others, since they had no symptoms or just minor ones. I have to add:
this situation requires a lot of patience from each member of society.
Dr. Krisztián Jáksó: Many people have expressed their gratitude in different forms: some of them brought us food, others wrote letters. What you or any member of society can do to express your thanks for the work of health care workers is to do anything in their power to minimise the risk of getting admitted to this department. If you follow the epidemiological guidelines, if you really stay at home, and minimize the risk of infection and cross-contamination, you can make our work easier. Many people have died all over the world, but not because the health care workers have been incompetent or the therapy has been medieval. Many of the of COVID-19 victims have died, because the explosive spreading of the infection has overloaded the healthcare system.
We are working here, so that the ones admitted can leave healed.
What is the best and the worst-case scenario?
Dr. Krisztián Jáksó: Best-case scenario is this current one; we have to stick to it. Unfortunately, the pictures of the highways around the Easter holidays have crushed my faith in this. The worst-case scenario is similar to the one in Italy. I have to add though that Hungary had and extra month to prepare. I think both our leaders and we all have used this time wisely.
Dr. Tamás Kiss: Social distancing should be the rule not only for a couple of weeks, but for months. This is a test of our mental strength, and one of its drawbacks is, that after a while people take it less seriously, because they are not aware of the danger. That Hungary had a lower infection rate in this pandemic from the beginning probably might play some role in this, and because of the precautions taken the number of patients is not extremely high – this also decreases the perception of fear.
Dr. Krisztián Jáksó: Some people are lacking a healthy sense of fear and responsibility. The 1918 Spanish flu has also been a “simple” influenza, but a certain type of it, which has not surfaced for decades before the pandemic. That pandemic needed two and a half years to travel around the Earth. Millions of people have died. Today, health care is much more advanced. However, there are major differences among the most endangered age groups of each country. The average life expectancy of Northern states is several years longer than that of Hungarians, and the health of an average person over 65 is also better in those states, compared to Hungary. We can tell ourselves that everything will be fine. I certainly hope that our society is more clever though, and nobody will be admitted to our unit because they have been careless.
Dr. Tamás Kiss: There is an anecdote about a Chinese specialist, who came to provide assistance in Italy, since he has been involved in the fight against the pandemic in Wuhan. He took a look at Milan, a city which the Italians thought was deserted and empty and he said: “This is not good. There are too many people on the streets.”
That the new case numbers are going down, does not mean that the pandemic is over, and there is no need for precautionary measures.

What kind of effect does the pandemic have on your lives now and later?
Dr. Tamás Kiss: My family supports me in everything, without them, I could not do my job well. I have three kids, one in secondary education, two in elementary school, they are all taking part in digital education at the moment. I have confess, the management of this falls to my better half. This situation bonds the family together, although it is difficult to convince a teenage girl that she cannot meet her boyfriend, and we keep in touch with the grandparents online only. It is hard to tell, what kind of changes the pandemic might bring in the future. Of course the outcome will be different, if we have to realize an almost unmanageable situation, or if it will not get worse than now. However,
we can feel a sense of professional pride, because we have set this unit up successfully.
Dr. Krisztián Jáksó: In the last couple of weeks we found ourselves in effective work relationships with certain people, with whom we would not ever have expected to work together, and several colleagues proved that they can outshine themselves. I do not want to be sentimental, but I have a 14 years old amazing and exceptionally intelligent daughter, who is taken care of by her mother at the moment, I live together with a beautiful woman, who is taking care of me. I have never participated in so many video conferences with my extended family before. Without a family background like this, it would be impossible to work like this.
I think we are learning to appreciate more, what we rarely noticed before.
Concerning the Centre: I think the people come here to work, knowing that they are safe, that we care about them, that they can work in calm surroundings along appropriate guidelines. It gives me a great sense of accomplishment, that we have successfully overcome every obstacle we had to face so far, including the protection of the health of our staff.

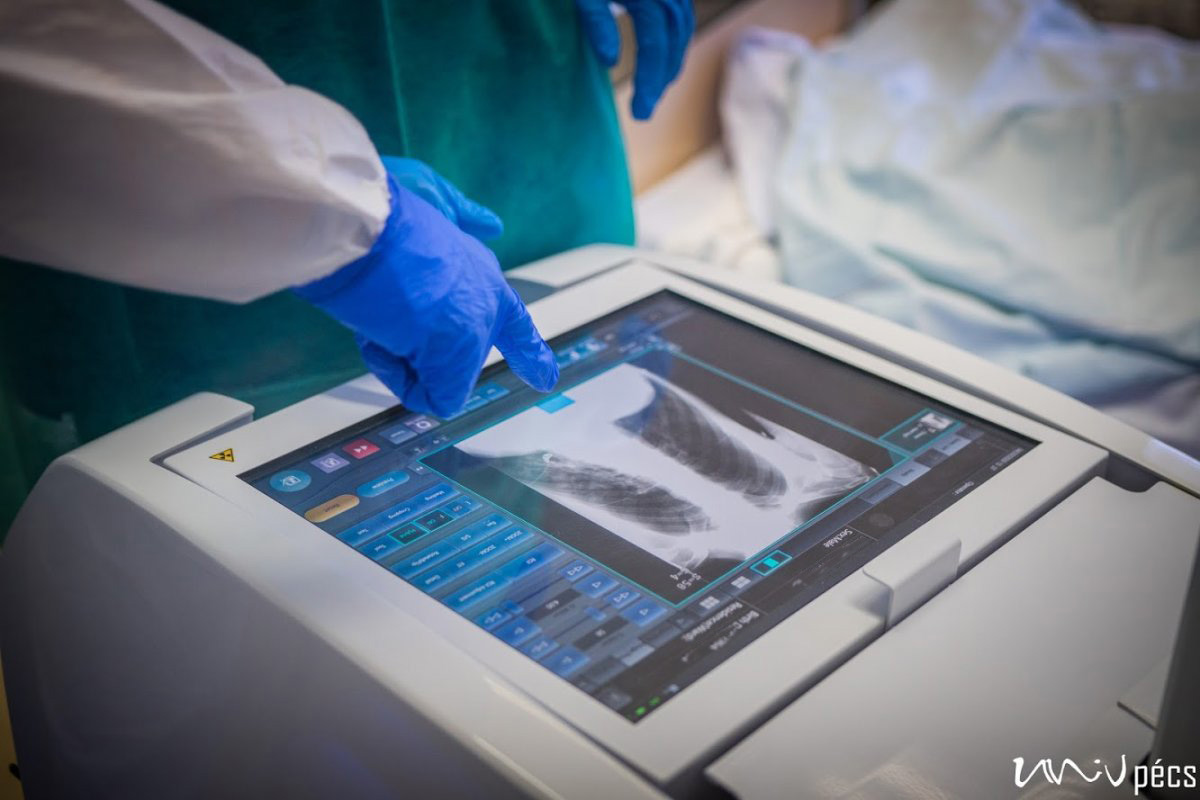
A security guard protects the entrance of building “C”, however, only very few people would volunteer to enter the top floor, where you can find the Coronavirus Care Centre Intensive Therapy Unit. Upon entrance, you arrive at a lounge area, where you have to take off all your street clothing. You have to put on disinfected socks, non-slip shoes and protective clothing. The COVID-ICU is divided into zones: you have disinfect everything you wear before and after entering the next zone. You can wear the same clothes in the green zone, in the yellow zone, you will need more serious protective gear. You have to put on an extra layer of shoe cover, gloves, scrubs/overalls, another layer of gloves, head cap, face mask, goggles, extra face shield if necessary. You have to check the protective gear before entering the next zone – this is why nobody can be alone! You are only allowed to enter the red zone after putting on the complete protective gear set. Here the patients are separated with glass walls – if there is a patient with a confirmed COVID-19 infection, their rooms are marked accordingly. In the rooms, there is negative pressure, meaning that if somebody enters the room, no air is going out of the room. It is forbidden to use air conditioning. The way out is different from the way in. The protective cover goes in the trash, followed by a thorough disinfection (you have to change your shoes as well). Before entering the yellow zone on the way out, all the clothing goes either in the trash or is disinfected. You can only enter the green zone in a completely new protective gear, masks and then after disinfection you can leave through the exit.
Protective gear is necessary, however, careful movement is recommended. If you have never tried to type in gloves before for example, you might have trouble imagining, what it is like to do anything that requires fine motor skills in double layer gloves. The double layer protective gear sticks to the skin underneath, if you take a large breath, even your goggles might turn foggy. Because not much of our face is visible behind the mask, head cap and goggles, you can only guess whether somebody is smiling or not. We hope that the least possible people have to guess.

by: UnivPécs
Photo: Szabolcs Csortos, UnivPécs
Read the original article (in Hungarian) »
- Log in to post comments
University of Pécs | Chancellery | IT Directorate | Portal group - 2020.





































































